Improving the HIV care cascade in Lesotho: Towards 90-90-90 – A research collaboration with the Ministry of Health
The 90-90-90 goals imply improved diagnostics and treatment for HIV-infected individuals. The project aims to link clinical and molecular research and infrastructural support with potential achievements to cut new HIV infections to a quarter.
About the project
Background
In November 2014 the Joint United Nations Programme on HIV/AIDS (UNAIDS) declared the 90-90-90 targets for 2020 as an intermediate step towards ending the AIDS epidemic as a global health threat by 2030. These targets are that 90% of HIV-infected individuals know their HIV-status, of these 90% receive sustained antiretroviral therapy (ART), and 90% of these achieve viral suppression. This will result in a suppressed viral load (VL) in 73% of all HIV-infected persons globally. The UNAIDS estimate that achievement of the 90-90-90 goal will facilitate a reduction of new HIV-infections from presently 2 million to below 500’000 per year in 2020. The rationale of the 90-90-90 targets lies in the preventive potential of ART. Mathematical modelling concludes that universal ART-coverage could indeed stop the epidemic. In line with the UNAIDS strategy, the World Health Organization issued in September 2015 the recommendation that anyone infected with HIV should begin ART as soon as possible after diagnosis.
Such a “test-and-treat” strategy bears, however, also unprecedented challenges to resource-limited settings where HIV is still hyper-endemic. The Continuum of Care Cascade (“the Cascade”) involves all steps HIV-infected individuals have to take in order to achieve viral suppression. It therefore starts at knowing the HIV-status, continues with linkage to care after a positive HIV-test, initiation of ART, uninterrupted continuation of therapy (called “retention in care”), and leads to viral suppression documented through regular VL monitoring. In Sub-Sahara Africa this care cascade is still far from the 90-90-90 targets. According to UNAIDS in 2013 only 45% of individuals were aware of their HIV-status, 39% of diagnosed individuals received ART and 29% of infected individuals had achieved viral suppression. In addition, diagnostic means are still largely missing that would allow the necessary virus monitoring. Innovative, effective, and practical approaches for improving the treatment cascade are thus urgently needed.
Lesotho, a small landlocked, impoverished country surrounded by South Africa has the second-highest HIV-prevalence in the world, the highest HIV transmission rates in the region and one of the lowest ART coverages in Southern Africa.
Objectives
The project involves operational, clinical and molecular research combined with infrastructural support, that jointly aim at improving the HIV care cascade towards reaching the 90-90-90 targets in Butha-Buthe, a district in Northern Lesotho. More specifically, observational and interventional studies address the following topics:
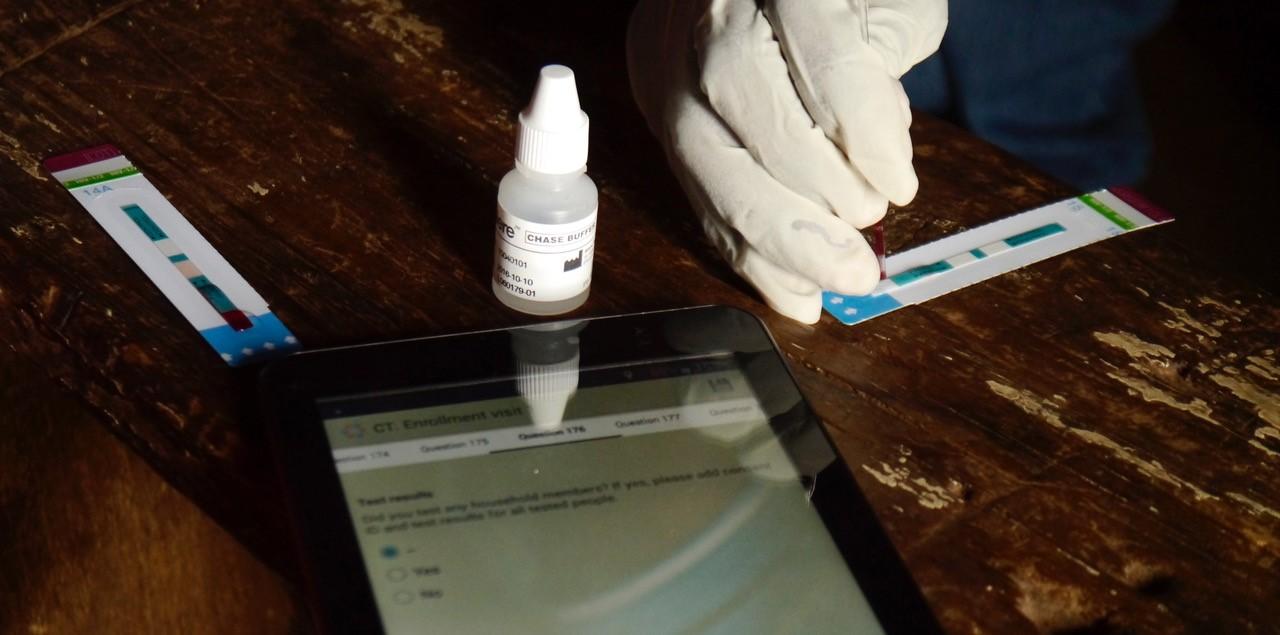
- Improvement of linkage to care, retention in care and viral suppression after home-based HIV testing and counselling (CASCADE-trial (NCT02692027)
- Roll-out of routine viral load monitoring and improvement of viral suppression among HIV infected individuals on antiretroviral therapy
- New approaches for HIV-infected individuals who fail first-line ART
- Establishing a molecular laboratory in Lesotho to conduct research on HIV resistance
- Capacity building among health care personnel in Lesotho.
Relevance
Impact is expected at the following levels:
- Improvement of the HIV care cascade in the district of Butha-Buthe
- Strengthened clinical, laboratory, and research capacity in Lesotho
- Generation of scientific evidence from a resource-limited hyper endemic setting to inform future national and international HIV policies and guidelines
Hightlights and most important results
Evidence for home-based same-day ART initiation
The CASCADE trial tested an approach to reduce loss of patients between HIV diagnosis, initiation of ART, and long-term engagement in care. A home-based testing and counselling campaign was carried out in 60 villages and 17 urban areas, visiting 6660 households. The campaign tested 11,590 adults, of whom 441 tested HIV positive. Of those who tested positive, 278 were willing and eligible to participate. The final analysis included 274 people, 76% female, with a median age of 39 years. Almost half (46%) had not been in contact with a health facility for at least a year, and half had to walk to the clinic. The median travel time to a clinic was one hour. The median CD4 cell count in study participants was 278 cells/mm3, and 16% had a CD4 cell count below 200 cells/mm3, indicating advanced HIV disease. Par- ticipants were randomized to receive either a 30-day supply of antiretroviral drugs on the day of diagnosis after home-based testing, or a referral to a medical facility to initiate antiretroviral therapy. The primary outcomes of the study were the proportion of participants in each arm who had linked to care within three months of diagnosis, and viral suppression below 100 copies/mL 12 months after diagnosis.
Same-day initiation resulted in significantly greater proportions linked to care within three months and virally suppressed 12 months later. 68.6% in the same-day arm and 43.1% in the standard-of-care arm linked to care within three months (P < 0.001). 50.4% in the in the same-day arm and 34.3% in the standard-of-care arm had suppressed viral load 12 months later.
The result of this trial was a proof of concept that reducing barriers to start ART after HIV diagnosis im- proves linkage to care. It did, however, not only look at linkage but at the proportion of patients still en- gaged in care with documented viral suppression 12 months after diagnosis (indicating successful therapy). Same-day ART did not only improve linkage but resulted in a substantially and significantly higher proportion of patients with viral suppression one year after diagnosis. This finding made the trial highly relevant for guidelines and policies.Findings of the CASCADE-trial were integrated into the following guidelines:
- USA guidelines: Antiretroviral Drugs for Treatment and Prevention of HIV Infection in Adults - 2018 Recommendations of the International Antiviral Society–USA Panel
- WHO guidelines: Guidelines for managing advanced HIV disease and rapid initiation of antiretroviral therapy
- By Feb 28, 2019, the publication of the CASCADE-trial has been cited in 18 peer reviewed articles, including policy-statements.
Routine Viral Load Monitoring
The project successfully set up the first decentralized molecular laboratory providing routine viral load monitoring in Lesotho. This laboratory based at Butha-Buthe Government Hospital serves two districts, Butha-Buthe and Mokhotlong. From Jan 1, 2016 to Feb 28, 2019, a total of 17,093 patients on ART had received overall 36,209 viral load measurements. More than 90% of ART patients in both districts had received at least one viral load measurement during the project period.
Geographic scope
- Lesotho
Links to project website and P3
- Link to project website (see also right column)
- Link to project on SNSF research database P3
